Connection Between White Blood Cells and Cancer
Connection Between White Blood Cells and Cancer
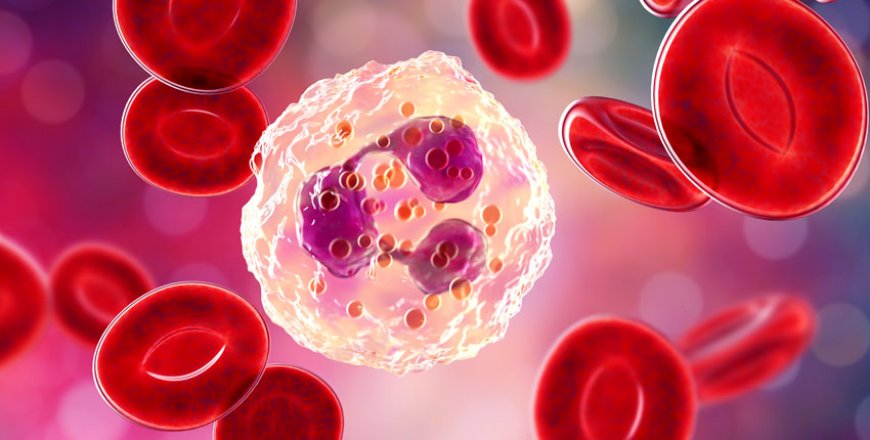
White blood cells (WBCs), also known as leukocytes, are pivotal guardians of our immune system. They detect, engage, and neutralize threats like infections, foreign particles, and even damaged cells. However, their relationship with cancer is multifaceted—and at times contradictory. While some white blood cells help control and eliminate tumors, others can paradoxically support cancer progression. This article explores the complex interplay between WBCs and cancer development, progression, and treatment. Along the way, we also touch on how pharmaceutical logistics—like Amoxicillin Wholesale sourcing and Azithromycin bulk supplier arrangements—impact the broader healthcare ecosystem.
1. White Blood Cells: Who They Are and What They Do
WBCs are diverse, each subtype with specialized functions:
-
Neutrophils: First responders, gobbling up bacteria and debris.
-
Lymphocytes: T cells and B cells orchestrate targeted immune responses; natural killer (NK) cells directly kill infected or aberrant cells.
-
Monocytes/Macrophages: Patrol tissues, ingest pathogens, and signal other immune players.
-
Eosinophils/Basophils: Involved in allergy, parasitic defense, and inflammation.
These cells routinely patrol our blood and tissues, maintaining surveillance and integrity. When healthy, they're effective cancer preventers; when dysregulated, they can enable tumor growth.
2. Immune Surveillance: WBCs vs. Cancer Cells
The immune system continuously surveys tissues, identifying and eliminating mutating cells. Key players include:
-
Cytotoxic T cells detect tumor-specific antigens and release toxic molecules (e.g., perforin, granzymes).
-
NK cells recognize 'altered-self' cells lacking normal MHC markers.
-
Macrophages can engulf tumor cells and present tumor antigens to T cells.
This “immunosurveillance” is highly effective—most nascent cancer cells are eliminated before causing harm.
3. Cancer’s Evasion Tactics
Cancer cells are notoriously crafty at evading immune detection:
-
Immune checkpoint expression: Many tumors express PD-L1, which binds to PD-1 receptors on T cells, causing immune paralysis.
-
Immunosuppressive secretions: Tumors secrete TGF-β, IL‑10, and other cytokines to create a local immune-suppressive microenvironment.
-
Recruitment of regulatory cells: Tumors attract regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs) that dampen adaptive immunity.
-
Antigen loss: Some cancer cells downregulate target antigens, making them invisible to T cells.
These adaptations highlight why immunotherapy (targeting PD-1/PD-L1, CTLA-4, etc.) has become such a promising treatment platform. By “releasing the brakes,” doctors can reignite white blood cell activity against cancer.
4. When WBCs Support Tumor Growth
Paradoxically, certain leukocytes sometimes aid tumors:
-
Tumor-associated macrophages (TAMs): Often adopting an M2-like, wound-healing phenotype, TAMs promote tissue rebuild, angiogenesis, and immune suppression.
-
Neutrophils: Some tumors hijack neutrophils to produce reactive oxygen species (ROS) and neutrophil extracellular traps (NETs) that help cancer spread.
-
MDSCs: These immature cells suppress T and NK activity and support new blood vessel formation.
Thus, cancer can twist white blood cells from defenders into unwitting allies.
5. Measuring WBCs and Cancer Prognosis
Clinically, certain white blood cell markers predict cancer outcomes:
-
Neutrophil-to-Lymphocyte Ratio (NLR): High NLR often signals poor prognosis across multiple cancers.
-
Elevated MDSCs or Tregs: Associated with aggressive tumors and therapy resistance.
-
Circulating tumor cells (CTCs) enveloped in leukocyte-“cloaks” show increased ability to metastasize.
These biomarkers help oncologists identify high-risk patients, tailor treatments, and track therapy effectiveness.
6. Harnessing WBCs for Treatment
Reprogramming white blood cells has transformed cancer treatment:
-
Checkpoint inhibitors: Therapies like pembrolizumab and nivolumab block PD-1/PD-L1, empowering T cells to attack tumors.
-
CAR‑T cell therapy: Patients’ T cells are engineered with a chimeric antigen receptor (CAR) to target specific cancer antigens—offering impressive results in leukemia and lymphoma.
-
Vaccines and cytokines: Interleukins (e.g., IL‑2) and GM‑CSF boost leukocyte activity.
-
Oncolytic viruses: These viruses kill cancer cells and stimulate a local immune reaction.
7. White Blood Cells in Combating Infection During Cancer
Cancer patients often face infection risk, due to immune suppression from the disease or its treatments (chemotherapy, radiation). This is where antibiotics like amoxicillin and azithromycin play a critical role.
Hospitals, pharmacies, and clinics rely on structured supply chains to access these medications:
-
Amoxicillin Wholesale channels supply large quantities of a front-line antibiotic for bacterial prophylaxis in neutropenic cancer patients.
-
Azithromycin bulk suppliers ensure availability of broad-spectrum agents for respiratory or other bacterial infections.
Maintaining reliable access reduces delays in treatment and improves patient outcomes during vulnerable periods.
8. The Intersection: Infection, WBCs, and Cancer Therapy
-
Neutropenic febrile episodes: Patients with low neutrophil counts (a result of chemo or bone marrow failure) develop fevers as a sign of infection. Guidelines recommend prompt empiric antibiotics—often including amoxicillin, azithromycin, or intravenous alternatives.
-
Prophylactic antibiotics: In select high-risk patients, oral amoxicillin or azithromycin may be used to prevent respiratory or skin infections.
-
Targeted therapy side effects: Some newer anticancer drugs raise infection risk, necessitating coordinated antibiotic supply.
Here, Amoxicillin Wholesale and Azithromycin bulk supplier partnerships segment supply chains so oncologists and pharmacists have timely, cost-effective access to critical medications—and patients receive prompt infection treatment.
9. Future Insights: White Blood Cells, Cancer, and Treatment Innovation
Ongoing research seeks to enhance therapeutic synergy:
-
Neutrophil engineering: Investigational therapies are converting neutrophils into targeted drug carriers to tumor sites.
-
Targeting TAMs/MDSCs: Treatments aimed at diminishing pro-tumor white cells or reprogramming them toward tumoricidal phenotypes.
-
Combined regimens: Antibiotics with immune-modulating properties—like azithromycin’s mild anti-inflammatory effects—are being tested alongside immunotherapy or chemo.
-
Microbiome modulation: Recent studies suggest gut flora—and the antibiotics we use—can shape immune responses to cancer and alter outcomes.
10. Take‑Home Messages
-
White blood cells are double‑edged swords: They can both combat and support cancer, depending on environmental cues.
-
Modern cancer care depends on precise immune modulation—via checkpoint inhibitors, CAR‑T therapies, and macrophage targeting.
-
Managing infection risk is vital: Access to antibiotics like amoxicillin and azithromycin is a key part of safeguarding immunocompromised patients.
-
Efficient supply chains matter: An Amoxicillin Wholesale operation and reliable Azithromycin bulk supplier network ensure clinicians aren’t hampered by shortages.
-
Research is accelerating: Next-generation strategies include white blood cell engineering, combined antibiotic‑immunity therapies, and microbiome-immune editing.
Conclusion
White blood cells are central to cancer’s story—sometimes acting as potent defenders, other times manipulated accomplices. Modern medicine is learning to direct their power more precisely, leveraging the immune system to eradicate tumors while managing infection risk. A well-coordinated pharmaceutical supply chain—anchored by Amoxicillin Wholesale and Azithromycin bulk supplier partnerships—ensures essential antibiotics are available to support these complex therapies. As research propels forward, the future promises smarter immune-guided treatments, better stewardship of infection risk, and new ways to harness (or restrain) white blood cells in the battle against cancer.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0


































