Medication for Panic Attacks - A Key to Regaining Control
Choosing the right medication for panic attacks involves collaboration between the individual and their healthcare provider.
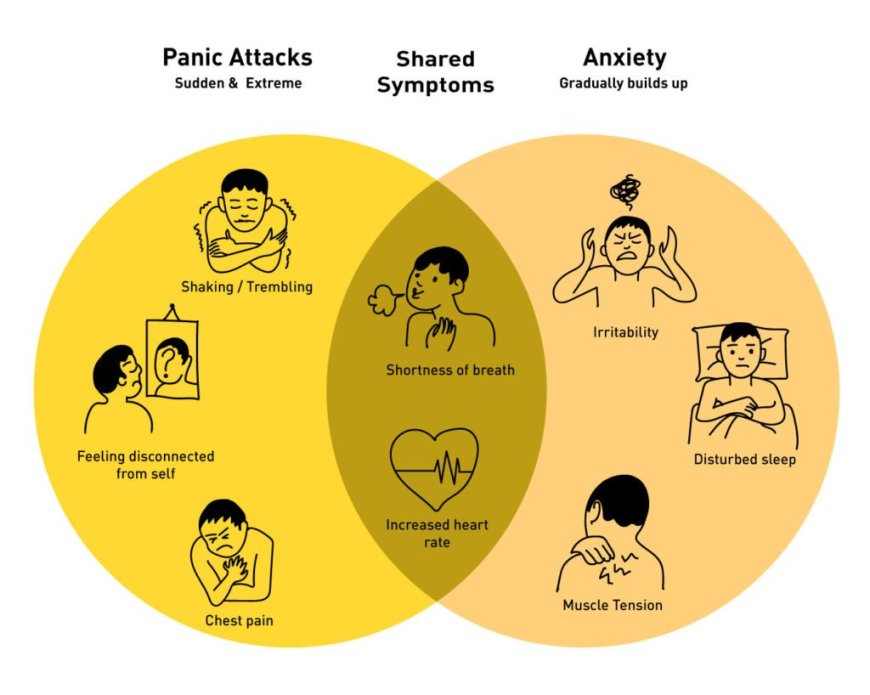
A panic attack is an isolated episode of anxiety or fear, typically with symptoms of heightened physiological response, including palpitations, chest pain, breathlessness or lightheadedness. Such episodes can be extremely distressing and may be particularly disabling, affecting most aspects of functioning. In those who experience frequent or severe panic attacks, pharmacological interventions may be required as part of the treatment program. Medication for panic attacks helps manage symptoms, reduce frequency, and restore a sense of normalcy.
Types of Medication for Panic Attacks
Several groups of drugs are usually administered in case of panic attacks. Both act differently; the method of taking depends on the patient's complaints, medical history, goals set for this therapy.
1. Selective Serotonin Reuptake Inhibitors (SSRIs)
Most of the time, SSRIs are used as the initial treatment for the management of panic disorder. These drugs help to raise levels of serotonin in the brain, which is crucial in the management of moods and anxiety. Common SSRIs include:
- Sertraline (Zoloft)
- Fluoxetine (Prozac)
- Paroxetine (Paxil)
While SSRIs are a useful antidepressant medicine class which helps most patients, it could take weeks to see some positive changes after surgery; it may contain side effects such as nausea, insomnia, and headaches that last for two weeks and may reduce with time.
2. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs are similar to SSRIs in that they help alter brain chemicals but also act on another brain hormone called norepinephrine. The specific SNRI is venlafaxine (Effexor XR), which is often used to treat panic disorder.
They are more effective than SSRIs and may be recommended for patients who experience poor outcomes with SSRIs. It also should be noted that this medicine may cause side effects like dizziness, dryness of the mouth, and elevation of blood pressure.
3. Benzodiazepines
Benzodiazepines are fast-acting medications that provide immediate relief during a panic attack. Common examples include:
- Alprazolam (Xanax)
- Clonazepam (Klonopin)
- Lorazepam (Ativan)
These medications treat the central nervous system, helping relieve symptoms such as tachycardia and hyperventilation immediately. However, they should not be taken long-term because the body becomes dependent on them, and they cause side effects such as drowsiness and memory loss.
4. Beta-Blockers
Propranolol (Inderal) is usually prescribed for the physical signs of panic disorders, for instance, tachycardia and tremor. They did not appear to be a long-term treatment for anxiety disorders but are effective for some situations, including public speaking or a specific /stressful occasion.
5. Tricyclic Antidepressants (TCAs) and Monoamine Oxidase Inhibitors (MAOIs)
For those who have not benefited from the use of SSRIs or SNRIs, the older classes of antidepressants, such as TCAs and MAOIs, can be considered. These are used less regularly since they have side effects and require the patient to adhere strictly to a special diet.
Combining Medication with Therapy
Although the medication helps to minimize the signs in many cases, it fails to provide the best outcome and is well-combined with therapy, for instance, CBT. CBT is handy when it comes to helping a person to make changes in ways that they think cause the onset of panic attacks, apart from medications.
Finding the Right Medication
Choosing the right medication for panic attacks involves collaboration between the individual and their healthcare provider. Safety and effectiveness of treatment depend upon medical history, current medications and other aspects of a patient's life. That is, time-to-time follow-ups assist in tracking the performance and determining dosage changes.
Moving Toward Stability
Choosing the right medication for panic attacks involves collaboration between the individual and their healthcare provider. Safety and effectiveness of treatment depend upon medical history, current medications and other aspects of a patient's life. That is, time-to-time follow-ups assist in tracking the performance and determining dosage changes.
What's Your Reaction?